A Q&A with Drs. Matthew Kalady and Steven Wexner
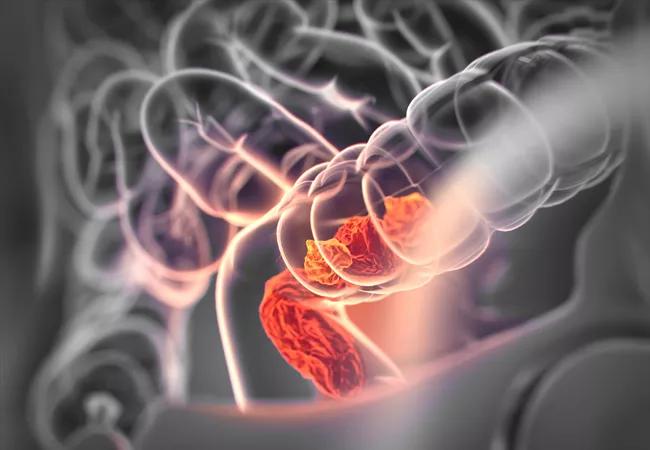
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b6b74979-0b5a-4106-89aa-1c27be6108f0/18-DDI-5519-Rectal-Cancer-Hero-Image-650x450pxl_jpg)
18-DDI-5519-Rectal-Cancer-Hero-Image-650x450pxl
The National Accreditation Program for Rectal Cancer (NAPRC) recently awarded its first accreditations to four of the nation’s top colorectal cancer programs, including the Cleveland Clinic Colorectal Cancer Program and the Cleveland Clinic Florida Colorectal Cancer Program.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
NAPRC accreditation – by the Commission on Cancer (CoC), a quality program of the American College of Surgeons – “is granted only to those programs that … undergo a rigorous evaluation and review of [their] performance and compliance with established NAPRC Standards,” according to the NAPRC.
Consult QD talked with colorectal surgeons Matthew Kalady, MD, Vice Chairman of Colorectal Surgery and Co-Director of the Comprehensive Colorectal Cancer Program, and Steven Wexner, MD, Director of the Digestive Disease Center and Chairman of Colorectal Surgery at Cleveland Clinic Florida and Past President of the American Society of Colon and Rectal Surgeons, about what the accreditation program means to patients and clinicians.
Dr. Kalady: We’ve long been a champion of multidisciplinary care with multiple specialties, with team agreement on optimal treatment plans. So, not much has changed in our daily practice. However, the accreditation affirms that we are consistent with best practices and helps us ensure that every single patient gets this standard of care.
We know outcomes are better at accredited centers for other conditions such as breast cancer, bariatric surgery and trauma. I think ultimately patients are going to seek care in centers that are accredited.
Dr. Wexner: The multidisciplinary approach and standardization remove personal prejudices that aren’t evidence-based. We think about a patient not just as surgeons or just as oncologists but collectively as members of a team. We achieve a better result when multiple minds are set to it, as research has shown that better approaches are found, irrespective of the experience of the surgeon. The wisdom of the group supersedes our individual opinions.
Advertisement
Dr. Kalady and our colleagues in Ohio proved this point. There are distinct benefits for patients when you consider the wisdom of the crowd. That’s number one. We are giving patients the greatest possible chance of surviving without a recurrence and without a colostomy.
Number two, it’s continuous learning for all the clinicians. When our specimens are put on a big screen and discussed among 40 or 50 people every week, we’ll naturally get much better. The collaborative teamwork among surgery, pathology, radiology, medical oncology and radiation oncology ultimately benefits our patients.
Dr. Kalady: We have emphasized efficiency of appointments and decreasing time to starting treatment. This process has pushed us to arrange clinic visits with multiple specialties on the same day and in the same space. After a complete evaluation is done, patients know that all the results are then discussed at our weekly cancer team meeting, and then the consensus recommendation is discussed with the patient. Patients really like the idea of getting the timely opinion of a full team.
Clinicians like it, too, because we all want to do the best for our patients and this gives us the opportunity to continuously improve what we’re doing. The medical community knows that six or seven years of effort went into this program, and it may well be a template for other cancers.
Advertisement
Advertisement
Strong patient communication can help clinicians choose the best treatment option
ctDNA should be incorporated into care to help stratify risk pre-operatively and for post-operative surveillance
The importance of raising awareness and taking steps to mitigate these occurrences
New research indicates feasibility and helps identify which patients could benefit
Treating a patient after a complicated hernia repair led to surgical complications and chronic pain
Standardized and collaborative care improves liver transplantations
Fewer incisions and more control for surgeons
Caregiver collaboration and patient education remain critical