Study supports a vasoconstrictive pathogenesis

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Reversible cerebral vasoconstriction syndrome (RCVS) comprises a group of diverse conditions characterized by reversible multifocal narrowing of the cerebral arteries heralded by sudden, severe (thunderclap) headaches with or without associated neurologic deficits and ‒ most importantly ‒ by reversible angiographic findings.
RCVS predominantly affects women and individuals in middle age. Presentation is usually dramatic, with patients describing their “worst ever” headache, which reaches its peak intensity in less than a minute. The headache usually involves severe to excruciating bilateral pain, starts posteriorly but generalizes quickly, and lasts anywhere from minutes to days. Interestingly, patients usually can identify a trigger for the syndrome, including strenuous exercise, sexual activity, coughing, sneezing or other Valsalva maneuver triggers, as well as other triggers, such as medications or drugs. RCVS is associated with subarachnoid hemorrhage in approximately 30 percent of patients and stroke in 40 percent.
Calabrese et al proposed the first diagnostic criteria for RCVS, which emphasize five points that must be fulfilled for a definitive diagnosis of RCVS:
Advertisement
RCVS is of major relevance to rheumatologists because it is the leading mimic of CNS vasculitis. Early recognition and diagnosis of RCVS can save patients the risks of unnecessary immunosuppression. Although the pathophysiology of RCVS is unclear, perturbations in the control of cerebral vascular tone are critical. The alteration in vascular tone observed in RCVS may be spontaneous or evoked by exogenous or endogenous factors, including exercise, emotional stress or drugs, among others. Given the profound and enduring implications of a diagnosis of CNS vasculitis, early recognition of its major mimic, RCVS, is critical since simple observation and support are often adequate for RCVS.
Little is known about the etiopathogenic basis of RCVS. It is widely accepted that a disturbance in the cerebral vascular tone is at the heart of the disease’s pathophysiology. This disturbance is hypothesized to be secondary to abnormal vascular receptor activity or sensitivity resulting from a spontaneous or evoked central vascular discharge. The disturbance also might be precipitated by the various endogenous or exogenous factors that have been associated with RCVS.
Clarifying the mechanisms and pathogenesis of RCVS falls squarely within the mission of Cleveland Clinic’s R.J. Fasenmyer Center for Clinical Immunology. By investigating biomarkers to aid in the diagnosis of RCVS and the development of therapeutic targets against it, we hope to better distinguish RCVS from other cerebral arteriopathies (both inflammatory and noninflammatory). This, in turn, may lead to reduced costs and morbidity, more effective diagnosis and, ultimately, the identification of appropriate therapies.
Advertisement
At the molecular level, it has been speculated that the many immunologic factors involved in subarachnoid hemorrhage-related vasospasm might be involved in RCVS as well. These include catecholamines, endothelin 1 (ET-1), serotonin, prostaglandins and nitric oxide.
Our group has taken a particular interest in the potential role of ET-1 in the pathogenesis of RCVS and recently reported a study comparing plasma ET-1 levels between RCVS patients and healthy controls. Endothelins are peptides secreted by vascular endothelial cells, and the most potent vasoconstrictor is ET-1.
Our study matched RCVS patients to healthy controls for race, gender and age and then compared ET-1 levels between the two groups. ET-1 levels were measured in RCVS patients both during an attack (ictal stage) and after resolution, and both levels were compared with control levels.
Significantly higher ET-1 levels were noted in RCVS patients compared with controls, and levels in RCVS patients showed a significant decline between the ictal and the resolution phases, the latter of which approached levels in controls. The table presents comparative ET-1 levels during the ictal stage of RCVS and in healthy controls.
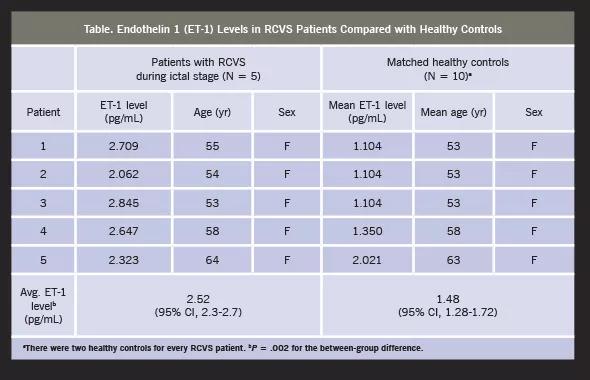
As speculated, these results ‒ both the elevated ET-1 levels during the ictal stage of RCVS and the decline in ET-1 after the resolution of vasoconstriction ‒ suggest a role for ET-1 in the pathogenesis of RCVS and endorse the vasoconstrictive pathogenesis of RCVS. We look forward to sharing additional results as our research on this topic progresses.
Advertisement
Dr. Hajj-Ali, who led the study reported here, is a staff physician in the Center for Vasculitis Care and Research and the R.J. Fasenmyer Center for Clinical Immunology in Cleveland Clinic’s Department of Rheumatic and Immunologic Diseases.
Advertisement
Advertisement

Treatment strategies require understanding of pathomechanisms

Education, prevention strategies and monitoring serves this at-risk group
Treatment for scleroderma can sometimes cause esophageal symptoms

Lupus Clinic providers collaborate to advance treatment and understanding

Older Psoriasis Patients May Experience Quicker Transition

Cleveland Clinic’s Rheumatic Lung Disease program treats patients with complex conditions

Symptoms complement one another

E-coaching program is tailored for those with the disease