Initiatives cover everything from STS performance metrics to facility renovations

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b0d4f3e8-2f6b-4a8d-bed3-57ec688a38d8/20-HVI-1917081-CQD-MedStar-Union-Hero_jpg)
20-HVI-1917081-CQD-MedStar-Union-Hero
Since the inception of MedStar Union Memorial Hospital’s alliance with Cleveland Clinic’s Miller Family Heart, Vascular & Thoracic Institute in 2013, the Baltimore-based hospital has undertaken numerous collaborative endeavors related to quality improvement and strategy implementation. Focus areas have included increasing productivity and efficiency, improving workforce utilization and implementing cost containment strategies. Additionally, MedStar Union Memorial Hospital (MUMH) has embarked on a journey with Cleveland Clinic to improve the overall quality of care it delivers to its local community.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This article profiles two initiatives carried out under the MUMH-Cleveland Clinic alliance, each demonstrating how the collaboration serves to support MUMH’s strategic goals and dedication to continuously enhancing patient safety.
Appropriate ventilator weaning and extubation following cardiac surgery decreases the risk for postoperative complications. Accordingly, risk-adjusted postoperative prolonged intubation (prolonged ventilation) is an established performance metric in the Society of Thoracic Surgeons (STS) Adult Cardiac Surgery Database. The metric represents the percentage of patients undergoing cardiac surgery who require intubation for more than 24 hours after exiting the OR. Upon initial assessment by Cleveland Clinic, MUMH’s prolonged ventilation rates were above national benchmarks and not consistent with MUMH’s strict standards for quality care.
To improve this metric, MUMH enlisted Cleveland Clinic postoperative clinical consultants to do the following:
Through monthly work plan calls, annual on-site evaluations of postoperative care and quarterly STS data analysis, a continuous improvement plan was developed and implemented by MUMH in collaboration with Cleveland Clinic consultants. In addition to addressing issues such as handoff communications and education of the postoperative care team, the plan revised multidisciplinary rounding practices. It also instituted real-time tracking of the prolonged ventilation metric to identify the primary reason(s) for failure to reach targets and to trend metric data over time.
Advertisement
The postoperative care team successfully modified their process for handoff communication between the OR to ICU teams to ensure discussion of mechanical ventilation weaning and extubation expectations as well as extubation-time goals, using guidance from existing respiratory therapy protocols. The formats of daily multidisciplinary rounds and nurse-to-nurse handoff reports were modified to raise awareness of how much time remained before a patient would exceed 24 hours of intubation and to prompt development of a patient-specific plan for liberation from mechanical ventilation if appropriate.
Implementation of these recommended practices and real-time data tracking was associated with a 69% relative improvement in rates of prolonged ventilation among patients undergoing any cardiac surgery procedure, from 16.3% at the start of the initiative in Q1 2015 to 5.1% in Q2 2019 (Figure).
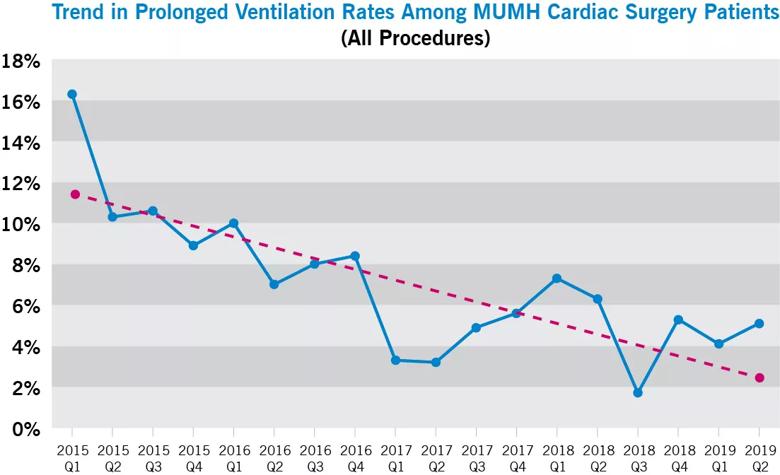
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e4d624d8-13a4-4051-8e04-f5b47f738082/20-HVI-1917081-CQD-MedStar-Union-Chart_jpg)
Figure. Rates of prolonged ventilation over time for MUMH patients undergoing all categories of cardiac surgery (coronary artery bypass grafting [CABG], valve, combined valve/CABG, other).
“Our team enjoys working with the Cleveland Clinic group,” says Cheryl Lunnen, Vice President, MedStar Heart & Vascular Institute at MUMH. “They are clinicians who understand real operational issues experienced by the staff, and together we come up with working solutions. Decreasing the extubation rate is just one example.”
In the fall of 2018, the MUMH cardiovascular medicine administrative team started reviewing plans to renovate two of their electrophysiology (EP) labs to make them more up to date. For help, they looked to Cleveland Clinic’s Section of Cardiac Electrophysiology and Pacing to review their blueprints and equipment list prior to the renovation. In the past 10 years, Cleveland Clinic has renovated six of the eight EP labs on its main campus, so the MUMH team welcomed the opportunity to tap their recent experience. Through emails and conference calls, key insights and recommendations were provided on the renovation plans and equipment needs of the new laboratories. Specific recommendations were wide-ranging, addressing issues such as fluoroscopy software, surgical lighting packages and placement, boom placement and mapping equipment software.
Advertisement
The MUMH team found the recommendations extremely helpful and reported that they reduced MUMH’s construction and equipment costs (see photos below from the renovated labs). “Working with Cleveland Clinic allowed us to create EP labs that were completely redesigned from the originals,” says MUMH’s Lunnen. “Because we had their expertise, minimal changes were necessary in construction and we now have labs that will take us into the future.”

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4cf6877e-5d28-4f54-8da4-86634293576c/20-HVI-1917081-CQD-MedStar-Union-Inset-2A-805p_jpg)

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b1e179f8-feaa-4465-bad9-8cd0f601e00f/20-HVI-1917081-CQD-MedStar-Union-Inset-2B-805p_jpg)
Photos from the renovated MUMH electrophysiology labs.
“The initiatives described above are examples of the many projects initiated and completed over the past seven years by MUMH and Cleveland Clinic’s Heart, Vascular & Thoracic Institute (HVTI) Strategic Operations Affiliate/Alliance Team,” says Suma Thomas, MD, MBA, Vice Chair, HVTI Strategic Operations at Cleveland Clinic. “We are engaged in a collaborative partnership that approaches complex issues in a transparent and efficient manner. Whether working on clinical or nonclinical projects, the affiliate/alliance relationship enables hospital teams to use their resources and past experiences to facilitate change and provide superior patient care.”
“Using industry-proven continuous improvement techniques such as Lean Six Sigma, our team of consultants leverages their deep knowledge and experience to provide alliance hospitals like MUMH with well-rounded recommendations in a variety of areas,” adds Edward Soltesz, MD, MPH, Director of Cardiac Surgery Affiliate and Alliance Programs. “These detailed insights yield actionable efforts to drive down cost while improving quality, patient flow and overall service line excellence.”
Advertisement
For information on affiliation and alliance opportunities with Cleveland Clinic’s Heart, Vascular & Thoracic Institute, visit clevelandclinic.org/heartaffiliates or email HVI_Strategic_Operations@ccf.org.
Advertisement
Advertisement
A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy
Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation
Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable