Initial successes relieve TMJ and lower extremity pain
A collaborative multidisciplinary team at Cleveland Clinic is achieving encouraging success in relieving temporomandibular joint (TMJ) pain for an increasing number of patients, using a unique mandibular nerve block technique.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Jianguo Cheng, MD, PhD, of the Anesthesiology Institute, and Joseph Krajekian, MD, DMD, of the Head & Neck Institute, devised this approach to help reduce the number of patients who need to have a joint replacement by Dr. Krajekian.
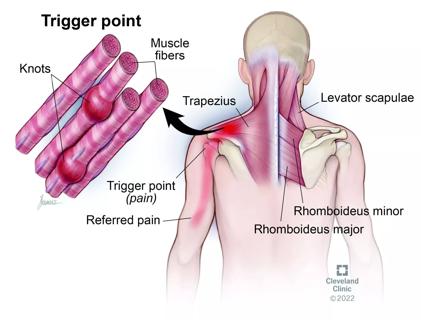
“Most patients with TMJ pain do not have a major structural problem, but they are in debilitating pain,” says Dr. Cheng. “We are focusing on helping this population.”
He describes the procedure as having two steps:
“To our surprise, most people do not need the second step, although some need to have the nerve block repeated in six to nine months,” says Dr. Cheng. “If the block is only effective for about two weeks, then those patients need to move on to radiofrequency ablation.”
He and his colleagues presented their findings at the American Academy of Pain Medicine recently and hope to announce a large cohort of outcomes data in one to two years. He says it is exciting to see what a big difference this procedure makes in people’s lives.
“They are free from debilitating pain in their jaw, and from the headaches it causes,” he says. “Many of them gain their life back after only one block.”
Anesthesiology Institute researchers were involved with the testing of a dorsal root ganglion (DRG) stimulator designed to relieve lower extremity pain that is now pending approval by the U.S. Food and Drug Administration.
Advertisement
The stimulator technology (created by Spinal Modulation and now owned by St. Jude Medical) was tested in a 17-site study. Samuel Samuel, MD, of Cleveland Clinic’s Anesthesiology Institute, was the principal site investigator in Cleveland.
“The device mimics a pacemaker, but what’s new about it is that it targets the pain-generating structure in the spine – the dorsal ganglion,” he says. “It can target pain from the waist down very specifically. For example, we can treat just the left foot, or the left foot and the right groin, or the right knee and the left foot, which is difficult to cover with conventional spinal cord stimulation therapy.”
He says this would be useful in chronic pain after surgeries for hernias or knee replacement, for example, or for patients with complex regional pain syndrome or failed back surgery syndrome with predominant leg pain (among other uses).
Dr. Samuel and his colleagues implanted a standard spinal cord stimulator, technology that has been in use for 25 years, into a group of patients, and then implanted the DRG stimulator in one patient – one of only 72 people in the country to receive it. That patient is doing very well and is happy with her results, after suffering with pain in one foot for years, he says.
“The results are very encouraging,” Dr. Samuel says. “Several papers on it were presented in June at the International Neuromodulation Society meeting in Montreal. The hope is for FDA approval potentially by the end of 2015.”
Last winter, Nagy Mekhail, MD, PhD, of Cleveland Clinic’s Department of Pain Management, began enrolling patients for a double-blind, randomized, controlled study to ascertain whether stem cells can alleviate pain arising from degenerative intervertebral disks. Dr. Mekhail serves as principal investigator at Cleveland Clinic, one of 13 sites in the U.S. and Australia participating in the research.
Advertisement
“When intervertebral disks develop fissures, nerve endings can grow into these cracks and cause pain,” says Robert Bolash, MD, a collaborator on the project. Options for patients with diskogenic pain have been relatively limited, including spinal fusion surgery and artificial disk replacement. Other treatments include intradiskal electrothermal annuloplasty (IDET), where nerve endings are cauterized, and biacuplasty, a method that uses water-cooled radiofrequency to treat injured disks.
“For the last 70-plus years, pain management physicians have sought to destroy nerves that send pain signals,” says Dr. Mekhail. “With this research, we hope to change the paradigm by regenerating the lumbar disks to treat nonradicular low back pain.”
The study will enroll 100 patients with single-level diskogenic back pain. Researchers will inject stem cells into the injured disk and allow them to differentiate into the tissue. They will follow patients for one year, measuring pain relief in several ways:
Patients also will undergo MRIs to see if the treated disks have regained height, which is lost during fracture.
“This line of research truly represents something cutting-edge,” says Dr. Bolash. “It has the potential to be a very exciting treatment, which could be offered to patients who haven’t gotten relief with traditional methods.”
Advertisement
Advertisement

Two-hour training helps patients expand skills that return a sense of control

Program enhances cooperation between traditional and non-pharmacologic care

National Institutes of Health grant supports Cleveland Clinic study of first mechanism-guided therapy for CRPS

Pain specialists can play a role in identifying surgical candidates

Individual needs should be matched to technological features

New technologies and tools offer hope for fuller understanding
Pathophysiology, diagnosis, treatment and a COVID-19 connection

Clinical judgment is foundational to appropriately prescribing