What physicians and administrators should know

By Monica Deadwiler
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The Centers for Medicare and Medicaid Services is expected to reach a major milestone this year. Its annual expenditures are projected to cross $1 trillion. Yes, one thousand billion dollars will be spent this year by the federal government on healthcare, a growth of $250 billion dollars from just five years ago. The factors that predominantly account for increases in healthcare expenditures are:
Bundled Payments for Care Improvement (BPCI) in the Medicare population, like BPCI Classic and BPCI Advanced, are primarily aimed at controlling the use and intensity of services. A bundled payment is an advanced payment model that combines the services of historically disparate areas of our healthcare system into a single bundled price for a defined clinical episode. This clearly aligns incentives, both clinical and financial, in such a way that should enable better outcomes all while controlling if not reducing the total cost of care. A bundled payment affords an opportunity for healthcare providers to organically grow revenue beyond the traditional fee-for-service payment model for the patients that we already see and treat.
Starting on October 1, 2018, CMS will transition providers from the voluntary BPCI Classic model into the BPCI Advanced model. BPCI Advanced spans 32 clinical episodes with a 90-day post-acute period, and clearly ties the positive or negative performance-based payments to quality. Below are my five key takeaways for this new model.
Advertisement
With 32 clinical episodes to choose from, providers must carefully consider how they will redesign their care across all 90 days for the patient, the payor and themselves when transforming care. Depending upon your organizations’ composition and preference, specialty strategies, population health management strategies or a hybrid may be the most effective to optimize care delivery.
Advanced care planning is making clear decisions about the care you wish to receive should you be unable to speak for yourself. While historically our systems, clinical and financial, are designed for caregivers to go extraordinary measures to save every patient at all costs, Medicare is signaling that systems need to be challenged, end-of-life care needs to be discussed and honoring patients’ preferences improves the family’s experience and care team’s resilience.
You can measure just about anything in a system. We know that data is king in healthcare, but robust, accurate and timely documentation of the healthcare services that are rendered to a patient will directly impact the data that is generated. Just like grooming a prince into a king, we need to thoughtfully focus on the documentation of our services that will ultimately become our data.
The descending order of the attribution hierarchy is that the patient is primarily attributed to one of three episode initiating groups: the attending physician in the physician group practice, then the operating physician and finally the hospital itself. In this program, CMS has sent a clear signal that the physician is responsible for the care for their patient both in the hospital and outside of it.
Advertisement
Mandatory CJR Metropolitan Statistical Areas (MSA) will take priority over BPCI Advanced. Regardless of your desire to participate in the Major Joint Replacement of the Lower Extremity clinical episode in BPCI Advanced, CMS’ mandatory CJR model will supersede a provider’s opportunity to participate in BPCI Advanced.
Regardless of one’s intent to participate in BPCI Advanced, the principles of population health management, advanced care planning and documentation accuracy apply across many value-based healthcare models and patient populations.
To learn more about the BPCI Advanced Model, connect with me at this year’s Cleveland Clinic Advanced Payment Summit. We have gathered a group of experts to share their successes and lessons learned along the way.
Monica Deadwiler is Senior Director of Healthcare Payment Innovation at Cleveland Clinic.
Advertisement
Advertisement
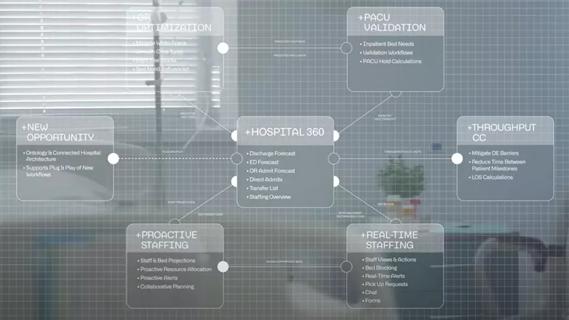
Cleveland Clinic partners with Palantir to create logistical command center

A Q&A with organizational development researcher Gina Thoebes

Cleveland Clinic transformation leader led development of benchmarking tool with NAHQ

Raed Dweik, MD, on change management and the importance of communication

Small business owners expand their networks and gain new insights

Leadership pearls from Margaret McKenzie, MD, hospital vice president

Advice from four CNOs on how to embrace innovation and collaboration

Cleveland Clinic will offer rapid, pinpoint airborne transport of medications and other medical items