From transcatheter replacement to new devices for easing repair

The rise of robotically assisted procedures is big news in mitral valve repair these days (see “RELATED” posts below), but it’s certainly not the only development in mitral valve surgery worth keeping an eye on.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cleveland Clinic cardiothoracic surgeons have played a lead role in the development and testing of several new and emerging technologies to make mitral valve surgeries less invasive and/or easier and more efficient. Three prime examples are profiled here.
RELATED: Robot-Assisted Repair Yields Robust Success in 1,000-Case Mitral Valve Series
Cleveland Clinic spinoff company NaviGate Cardiac Structures recently announced the first-in-human implant of its stented transcatheter mitral valve prosthesis into a beating heart.
The investigational device was developed by Cleveland Clinic cardiothoracic surgeon José Navia, MD, and licensed to NaviGate in 2012. It is among the first experimental systems designed for catheter-based mitral valve replacement and offers the following innovative features:

Figure 1. The NaviGate stented transcatheter mitral valve prosthesis.
The first human implantation was performed in Chile in October 2015 in a 53-year-old man with severe mitral regurgitation as part of a feasibility study. The prosthesis was successfully placed in the mitral position via transatrial delivery. The patient has fared well, with no paravalvular leakage and no outflow tract obstruction.
Advertisement
Despite high hopes for transcatheter mitral valve replacement approaches like the NaviGate prosthesis for use in inoperable patients, repair is still considered the best option for most patients who require mitral valve procedures.
“A valve replacement gets you a top grade of A,” says Cleveland Clinic cardiothoracic surgeon A. Marc Gillinov, MD. “But if you can get your own valve repaired and it works, that’s an A+. Replacement is not bad, but in general, especially for prolapse, repair is preferable.”
To that end, Cleveland Clinic surgeons have been working closely with industry partners to develop devices to make mitral valve repair easier and more efficient. Among their projects is the FDA-approved and recently launched Chord-X™ Mitral Valve Chordal Repair System (Figure 2), which makes it easier for surgeons to accurately measure the length of the chords that connect the mitral valve leaflets to the walls of the left ventricle and then adjust or create customized chordal loop lengths.
“This technology helps simplify and standardize chordal replacement during mitral valve repair, which shortens the patient’s time in the operating room,” Dr. Gillinov notes.
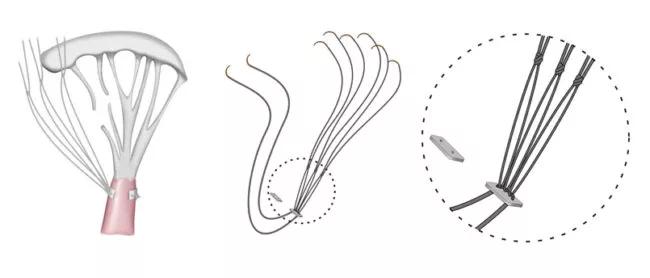
Figure 2. Illustrations showing how the Chord-X system works. Images used with permission from On-X Life Technologies, Inc.
RELATED: Managing Mitral Valve Disease in 2016
An additional repair-related innovation that Cleveland Clinic cardiothoracic surgeons helped develop is an experimental intravalvular balloon device called Mitra-Spacer™, which promises another potential option for patients not eligible for surgical treatment.
Advertisement

Figure 3. The Mitra-Spacer™. Image courtesy of Cardiosolutions, Inc.
This reversible implantable device is inserted between the mitral valve leaflets to fill the gap between them that gives rise to mitral regurgitation. The inflatable, balloonlike Mitra-Spacer can be delivered via a transapical or transseptabl approach and is tethered to the base of the left ventricular apex by a chord (Figure 3). It does not alter the anatomy but provides a sealing surface for the leaflets with the aim of reducing or eliminating regurgitation.
“It’s in clinical trials and we’re very optimistic about it,” says Dr. Gillinov.
Top image courtesy of Cardiosolutions, Inc.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable